Blogs

Types of Tendonitis in the Foot

Tendonitis, inflammation, and irritation of tendons are common causes of foot pain. Tendonitis can lead to acute pain, swelling, and tenderness that may inhibit mobility. Various types of foot tendonitis can occur, each with distinct characteristics and causes. Achilles tendonitis, for instance, affects the Achilles tendon, commonly occurring a few inches above the heel where the tendon is weakest. Extensor tendonitis involves inflammation of tendons running along the top of the foot, often the result of friction from wearing ill-fitting footwear, particularly affecting individuals with high arches. Flexor tendonitis, prevalent among dancers and those requiring frequent toe balancing, induces deep ankle pain near the inner foot. Peroneal tendinosis, affecting tendons wrapping around the outer foot and ankle, leads to pain and swelling. Posterior tibial tendonitis, commonly associated with flat feet, causes pain and swelling along the inside of the foot due to inflammation of the tibialis posterior muscle tendon. An effective treatment plan may involve rest, orthotics, or other interventions. If you are experiencing pain from any foot-related tendonitis, it is suggested that you schedule an appointment with a podiatrist for an exam, diagnosis, and treatment options.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with David Lambarski, DPM from Northeast Foot Care. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in Amsterdam and Clifton Park, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your foot and ankle doctor to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.
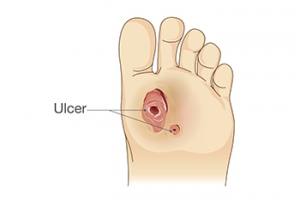
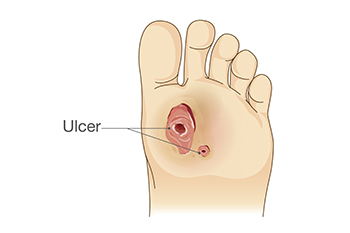
How Podiatrists Manage Diabetic Feet
 Podiatrists play a vital role in diabetic foot care, offering specialized assistance to prevent foot complications from developing. People with diabetes need to pay close attention to foot care, because high blood sugar can cause damage to nerves and result in poor blood circulation in the feet. When people cannot feel pain in their feet, they may not notice problems such as cuts and ulcers. Wounds are at even higher risk for infection as a result of poor blood flow. Podiatrists help by conducting regular foot exams to identify any issues early on. They also perform neurovascular and musculoskeletal assessments for the feet. Podiatrists educate their patients about proper foot hygiene, nail care, and daily foot checks, as well as recommend suitable footwear to prevent problems. If a patient has foot issues such as calluses, corns, or ingrown toenails, this type of doctor can treat them to prevent the issues from worsening. If you have diabetes and suspect foot problems, it is suggested you consult a podiatrist who can help you manage and prevent foot-related complications due to having diabetes.
Podiatrists play a vital role in diabetic foot care, offering specialized assistance to prevent foot complications from developing. People with diabetes need to pay close attention to foot care, because high blood sugar can cause damage to nerves and result in poor blood circulation in the feet. When people cannot feel pain in their feet, they may not notice problems such as cuts and ulcers. Wounds are at even higher risk for infection as a result of poor blood flow. Podiatrists help by conducting regular foot exams to identify any issues early on. They also perform neurovascular and musculoskeletal assessments for the feet. Podiatrists educate their patients about proper foot hygiene, nail care, and daily foot checks, as well as recommend suitable footwear to prevent problems. If a patient has foot issues such as calluses, corns, or ingrown toenails, this type of doctor can treat them to prevent the issues from worsening. If you have diabetes and suspect foot problems, it is suggested you consult a podiatrist who can help you manage and prevent foot-related complications due to having diabetes.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact David Lambarski, DPM from Northeast Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our offices located in Amsterdam and Clifton Park, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Care
Diabetes can cause two problems that can potentially affect the feet: Diabetic neuropathy and Peripheral Vascular Disease. Diabetic neuropathy occurs when nerves in your legs and feet become damaged, which prevents you from feeling heat, cold, or pain. The problem with diabetic neuropathy is that a cut or sore on the foot may go unnoticed and the cut may eventually become infected. This condition is also a main cause of foot ulcers. Additionally, Peripheral vascular disease also affects blood flow in the body. Poor blood flow will cause sores and cuts to take longer to heal. Infections that don’t heal do to poor blood flow can potentially cause ulcers or gangrene.
There are certain foot problems that are more commonly found in people with diabetes such as Athlete’s foot, calluses, corns, blisters, bunions, foot ulcers, ingrown toenails, and plantar warts. These conditions can lead to infection and serious complications such as amputation. Fortunately, proper foot care can help prevent these foot problems before they progress into more serious complications.
Each day you should wash your feet in warm water with a mild soap. When you finish washing your feet, dry them carefully especially between your toes. You should also perform daily foot inspections to ensure you don’t have any redness, blisters, or calluses. Furthermore, if you are diabetic, you should always wear closed-toed shoes or slippers to protect your feet. Practicing these tips will help ensure that your feet are kept healthy and away from infection.
If you have diabetes, contact your podiatrist if you have any of the following symptoms on your feet: changes in skin color, corns or calluses, open sores that are slow to heal, unusual and persistent odor, or changes in skin temperature. Your podiatrist will do a thorough examination of your feet to help treat these problematic conditions.
Symptoms and Risks of Plantar Warts

Plantar warts, caused by the human papillomavirus, HPV, can develop in anyone, but certain factors may heighten vulnerability. Individuals with weakened immune systems are at an increased risk, as the body's defense mechanisms struggle to combat the viral invader. The symptoms of plantar warts often include small, fleshy growths on the soles of the feet, accompanied by tenderness or pain while walking. Children and teenagers, with developing immune systems, are particularly susceptible to these uncomfortable growths. Prolonged exposure to moist environments, such as communal showers or swimming pools, also escalates the risk. Additionally, those who frequently walk barefoot in public spaces may find themselves more prone to contracting the virus. If you have developed a plantar wart, it is strongly suggested that you visit a podiatrist who can offer effective treatment options and prevention tips.
Plantar warts can be very uncomfortable. If you need your feet checked, contact David Lambarski, DPM from Northeast Foot Care. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our offices located in Amsterdam and Clifton Park, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
All About Plantar Warts
Plantar warts are warts that are only found on the feet, hence the term “plantar”, which means “relating to the foot.” They are caused by the human papillomavirus, or HPV, and occur when this virus gets into open wounds on the feet. The warts themselves are hard bumps on the foot. They are easily recognizable, mostly found on the heels or ball of the foot. Plantar warts are non-malignant, but they can cause some pain, discomfort, and are often unsightly. Removing them is a common step toward treating them.
Plantar warts can cause some pain while standing, sometimes felt as tenderness on the sole of your foot. Unless the wart has grown into the foot behind a callus, you will be able to see the fleshy wart. A podiatrist should only be consulted if there is an excessive amount of pain. Plantar warts are not cancerous or dangerous, but they can affect your walking and continually reappear. Anyone who suffers from diabetes or a compromised immune system disease should seek out care immediately.
Podiatrists are easily able to diagnose plantar warts. They usually scrape off a tiny bit of the rough skin to make tiny blood clots visible and examine the inside of warts. However, a biopsy can be done if the doctor is not able to diagnose them from simply looking at them. Although plantar warts usually do not require an excessive amount of treatment, there are ways to go about removing them. A common method is to freeze them off using liquid nitrogen, removing them using an electrical tool, or burning them off via laser treatment. For a less invasive treatment option, topical creams can be used through a doctor’s prescription. This treatment method takes more time, however. Keep the wart covered for protection in between daily treatments.
The best way to avoid developing plantar warts is to avoid walking barefoot in public places. Avoid this especially if you have open sores or cuts on your feet. It is also important to avoid direct contact with warts in general, as they are highly contagious.
Common Reasons Why Feet Can Swell

Swollen feet, or edema, can disrupt daily life. This condition often has a spectrum of common causes that individuals should be attuned to for timely intervention and relief. Prolonged periods of standing or sitting, especially in positions that impede healthy blood circulation, can lead to fluid retention, resulting in swollen feet. Another frequent contributor is the choice of footwear, with ill-fitting shoes or high heels imposing pressure that hinders proper blood flow. Injuries, such as sprains or fractures, can trigger inflammation and swelling in the affected area. Underlying medical conditions, including venous insufficiency, arthritis, or heart failure, may manifest in swollen feet. Hormonal changes during pregnancy often result in fluid retention, causing noticeable swelling in the feet and ankles. Lifestyle factors, like a diet high in sodium, can exacerbate fluid retention. Swollen feet can be uncomfortable, and if you have this condition, it is suggested that you visit a podiatrist who can accurately determine the cause, and offer appropriate treatment tips.
Swollen feet can be a sign of an underlying condition. If you have any concerns, contact David Lambarski, DPM of Northeast Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Swollen feet are a common ailment among pregnant women and people who stand or sit for extended periods. Aging may increase the possibility of swollen feet and patients who are obese often notice when their feet are swelling too. There may be medical reasons why swollen feet occur:
- Phlebitis - A condition that causes the veins to become inflamed and can also cause leg pain.
- Liver disease - This may lead to low blood levels of albumin which is a protein. This can cause fluid in the blood to pass into the tissues and several areas of the body can become swollen.
- Heart failure - When the heart doesn’t pump properly the blood that is normally pumped back to the heart can pool in the veins of the legs causing swollen feet.
- Kidney disease - One of the main functions of the kidneys is releasing excess fluid in the body. This type of condition can make it difficult for the kidneys to function properly, and as a result the feet may become swollen.
- Deep-vein thrombosis (DVT)- This is a serious condition where blood clots form in the veins of the legs. They can block the return of blood from the legs to the heart which may cause the feet to swell. It is important to be treated by a podiatrist if this condition is present.
Swollen feet can also be caused by bone and tendon conditions, including fractures, arthritis, and tendinitis. Additionally, there may be skin and toenail conditions and an infection may cause the feet to swell. Patients who take medicine to treat high blood pressure may be prone to getting swollen feet.
Many patients elevate their feet to help relieve the swelling and this is generally a temporary remedy. When a podiatrist is consulted the reason behind the swelling can be uncovered and subsequently treated.
If you have any questions please feel free to contact our offices located in Amsterdam and Clifton Park, NY . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Swelling of the Feet
There are many reasons why patients experience swelling of the feet. It is rather common and may be a side effect of pregnancy or from sitting and standing for most of the day. Gravity could also play a role in the development of swollen feet. It is known that the weight of blood volume in our bodies is exerted on the veins in the legs and feet. The veins may not work as efficiently during the aging process, and this could make the blood flow backward causing swollen feet. Relief may be found when obese patients lose weight, and it may help to engage in compression therapy by wearing compression socks, stockings, or athletic sleeves. This method can release pressure on the feet and ankles which may help to reduce existing swelling. There are patients who have controlled their swollen feet by implementing healthy lifestyle changes. These can consist of reducing salt intake, incorporating a gentle exercise regime into the daily routine, and drinking plenty of fresh water. Swollen feet may be a temporary condition that affects people who travel via airplane or automobile, so it is beneficial to walk as frequently as possible even though it can be difficult. Swelling of the feet can also be indicative of other health issues so it is important to pay attention to any type of chest pain, mental confusion, dizziness, or fever. If you consistently have swollen feet, it is strongly suggested that you consult with a podiatrist who can help determine the cause and how to effectively treat it.
The Seriousness of Cracked Heels

Cracked heels, medically known as heel fissures, are more than just a cosmetic issue, they can be quite serious. These splits in the skin surrounding the heel can become deep and cause pain, especially while standing or walking. For some individuals, the cracks are superficial, but for others, they can lead to bleeding and infections, particularly in those with compromised immune systems. In addition, people who have conditions such as diabetes can impair healing, possibly increasing the risk of foot complications. The skin around the heels is often subjected to pressure and weight-bearing, and if it is not supple due to dryness or thickened due to calluses, it is prone to cracking. Factors contributing to this can include walking barefoot or wearing open-backed shoes, prolonged standing, obesity, and certain skin conditions. In severe cases, dead skin may need to be removed by a podiatrist and medication prescribed. If you have cracked heels that are not healing or are worsening, it is suggested that you make an appointment with this type of medical professional for prompt treatment.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact David Lambarski, DPM from Northeast Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our offices located in Amsterdam and Clifton Park, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.